
The diagnosis of "cervical osteonecrosis" is often made if a person complains of neck pain. Some people also attribute it to dizziness, memory loss, numbness in the hands and other unpleasant symptoms. It is mistakenly believed that the disease is related to age-related wear and tear of the intervertebral discs and other parts of the spine.
How does the cervical spine work?
The cervical region includes 7 vertebrae. Between them are the intervertebral discs - semi-rigid structures with a dense ring along the periphery and a jelly-like center that act as shock absorbers. On the right and left sides of each vertebra there are two joints, between which protrude the surfaces of the vertebral processes, covered with cartilage. The joints are connected by ligaments and back muscles.
Why does neck pain happen?
Typically, neck pain occurs due to inconvenient movement, injury, or inflammation of any structure of the cervical spine. In addition, the cause of pain can be excessive tension in the muscles or ligaments, for example, when lifting weights, unsuccessfully turning the head, or due to arthritis between the joint processes. "Nerve entrapment", or cervical radiculopathy, specific processes (metastases, vertebral tumors, spinal cord membranes in the cervical region) are relatively rare.
26% of men and 40% of women over 30 years old experienced neck pain in the past month, 5% of men and 7% of women always felt neck pain.
Acute neck pain usually resolves on its own within 1–2 weeks. Chronic pain in most cases appears due to lack of physical activity or, conversely, too intense exercise.
However, people often mistakenly refer to unexplained pain and discomfort in the neck as cervical cartilage degeneration and link its development to age-related wear and tear of the intervertebral discs and joints. other parts of the spine. But such pain, as a rule, has nothing to do with real osteonecrosis.
Cervical bone degeneration
According to the International Classification of Diseases (ICD), osteochondrosis (osteochondropathy) is a group of rare genetic diseases involving disruption of normal bone development and growth. As a rule, osteonecrosis begins in childhood and is severe: part of the joint or bone is deformed, sometimes even fatal. With this disease, it is often not the cervical spine that is affected, but the thoracic spine (lower thoracic vertebrae). Therefore, the main clinical manifestation of osteochondrosis is a pronounced curvature of the thoracic spine, also known as thoracic kyphosis.
Symptoms related to thoracic spine damage:
- shortness of breath,
- persistent weakness
- unable to breathe fully,
- pain and burning behind the sternum,
- attacks of tachycardia.
The condition is accompanied by neck pain
Cervical spondylosis
In people over 50 years old, neck pain is often caused by cervical spondylosis, age-related wear and tear of the vertebrae and related structures. With this disease, the intervertebral discs become dehydrated and collapse, causing more severe degeneration in the neck area, increased movement, and pain.

But changes in the spine as we age are normal. Therefore, its structures begin to wear out after an average of 30 years, and by the age of 60, 9 out of 10 people have cervical spondylosis. However, in most people, it has no symptoms.
Other reasons
Less commonly, neck pain occurs due to hypothermia or severe stress, due to herniated discs or abnormalities of the cervical vertebrae - bony growths (spurs) that compress the nerves extending from the spinal cordliving.
The most common cause of pain in the cervical spine and shoulder girdle is excessive tension in the (defensive) muscles: trapezius, long back muscles of the cervical spine.
In addition, the muscles of the cervical spine are closely connected to the aponeurosis - a wide tendon sheet that covers the head. The muscular components of the occipital, temporal and forehead muscles connect with the muscles of the neck, so neck pain is often accompanied by headaches. Therefore, neck pain that appears after sedentary work or sleeping in an uncomfortable position and combined with headaches, in most cases is associated with lack of physical activity, incorrect postureand does not pose a health hazard.
The phenomenon of tech neck, also known as tech neck or Internet neck, is related to pain that arises from uncomfortable posture. Techneck is the result of constant use of computers and smartphones, due to which a person is forced to bend his or her neck. In fact, the relative mass of the head increases when tilted forward. Thus, in a "straight" position, the average weight of an adult's head is 5 kg. If you tilt your head forward at least 15°, then the load on the neck muscles will be 13 kg, at an angle of 30° - 20 kg, at an angle of 60° - 30 kg. Due to constant overload, the neck muscles become overstretched, microtrauma, inflammation, fibrosis (connective tissue overgrowth) and, as a result, pain may occur.
Causes that contribute to the development of cervical spine degeneration
The appearance of pain in the cervical spine is facilitated by birth or any other injury of the spine, abnormalities in its development, disorders of posture, dystonia, as well as prolonged immobility, obesity, and some autoimmune diseases.
- Long-term immobility is a condition in which a person, due to a pre-existing condition, is forced to lie down for more than a month. As a result, the muscles weaken - and during uprighting, as the load on them increases, they become excessively tense. Pain occurs.
- Obesity: Excess body weight increases stress on spinal structures and can cause pain.
- Autoimmune diseases in which cartilage tissue is destroyed (autoimmune arthritis, polychondritis) also lead to neck pain.
Stages of cervical spine degeneration
There are 4 main stages of degeneration (destruction) of the cervical spine:
- Phase I: the intervertebral disc becomes thinner, a slight feeling of discomfort appears in the neck area;
- Phase II: the disc is deformed, the distance between the vertebrae is reduced. Pain increases with movement in the cervical spine;
- Phase III: Cartilage and vertebrae rub against each other, neck pain is constant and movement becomes limited. With very severe deformities of the cervical spine, vertebral artery syndrome may occur, accompanied by visual and vestibular disorders and headaches;
- stage IV: clear degeneration, movement in the cervical spine is very limited and painful. The neck area may be almost completely immobile.
Symptoms of cervical spine degeneration
Most people with cervical spondylosis have chronic pain and neck stiffness. As the disease progresses, other symptoms may appear (especially if the spinal roots, vertebral arteries and neighboring nerve plexuses are compressed).
Signs of cervical spine degeneration:
- neck pain that gets worse with movement or standing;
- pain spreading to the shoulder or arm;
- numbness, tingling, and weakness in the arms and hands;
- clicking or grinding in the neck (especially when turning the head);
- headache;
- dizziness;
- impaired ability to coordinate movements;
- loss of bladder or bowel control.
If such symptoms appear, you should consult a neurologist as soon as possible.
Types of symptoms of cervical spondylosis
All symptoms of "cervical spondylosis" can be conditionally classified into 3 groups or syndromes: vertebral, root and vertebral artery syndromes.
Symptoms of vertebral (spine) syndrome:
- crunching sound in the neck when moving;
- limited mobility;
- violation of the position of the vertebrae relative to each other in the neck;
- flattens natural torticollis or lateral curvature in the cervical spine (visible only on X-ray, MRI or CT).
Symptoms of root syndrome:
- numbness of fingers in one or both hands;
- shooting, burning pain in the neck, spreading to the arm or both arms;
- neck and arm muscular dystrophy.
Symptoms of vertebral artery syndrome:
- paroxysmal vertigo, leading to loss of consciousness;
- sudden increase in blood pressure;
- noise in the ears;
- blurred vision or spots in the eyes;
- loss of balance and nausea when moving the head;
- headache (severe pain on one or both sides).
Diagnosis of degenerative changes in the cervical spine
To understand the cause of neck pain and diagnose "cervical spondylosis" (often called cervical spondylosis), your doctor will need to conduct an examination, study your medical history, evaluate test results, and examine you. tool. .
The diagnosis and treatment of cervical spondylosis is performed by a neurologist.
Investigate
During the examination, the doctor will listen to the patient's complaints, clarify the medical history in detail and conduct an examination: check reflexes, muscle strength, sensitivity, condition of the vestibular apparatus.
With "cervical cartilage degeneration", areas of muscle atrophy (muscle loss) are visible, the muscle tone of the long back muscles is reduced or increased, and static disorders of the neck can be observed. . When palpating the muscles, the patient complains of pain. When tilting the head, the pain may spread to the head or arm, dizziness or headache may occur.
In addition, patients may experience hand movement disorders (weakness), vision and hearing problems.
The doctor may also ask the patient to walk, stand on one leg and close their eyes or touch their nose. In this way, the specialist will be able to assess whether the coordination of movements is impaired, whether there are problems with gross and fine motor skills.
Laboratory diagnosis
To assess the general condition of bones, patients suspected of having cervical spondylosis are prescribed blood tests for total and ionized calcium, as well as markers of bone tissue growth and destruction - Osteocalcin andOsteoprotegerin, alkaline phosphatase.
As cervical cartilage degeneration progresses, joints are destroyed, calcium content may decrease, on the contrary, Osteocalcin and Osteoprotegerin increase.
Total creatine kinase is also considered a marker of muscle tissue destruction in cervical myositis.
Additionally, your doctor may need to assess blood levels of trace elements involved in regulating muscle tone: magnesium, potassium, sodium.
Diagnostic tools
To determine the cause of neck pain and related disorders, imaging studies are required: cervical spine radiography, computed tomography and magnetic resonance imaging, and electromyography.
- X-ray.Using X-rays, you can identify bone deformities, malignant tumors and degenerative changes in the joints.
- Magnetic resonance imaging and calculationsperformed if disease of the spine, spinal cord, or brain is suspected. Computed tomography showed hemangioma in the vertebral body and severe deformities of the cervical spine. Magnetic resonance imaging provides more information for visualizing the muscles, roots, and spinal cord.
- Electroencephalography- method of studying the efficiency of impulse transmission along nerve fibers using low-intensity electric current. Testing can be a bit uncomfortable. Research helps clarify the conduction of impulses along roots, nerves and from nerves to muscles, confirm damage to nerves or muscles and clarify the nature and extent of damage.
Treatment of degenerative changes in the cervical spine
The main goals of treating degenerative changes in the cervical spine are to relieve pain, prevent nerve compression in the neck, and restore neck mobility.

Depending on the severity of the condition, your doctor may prescribe medication, physical therapy, or massage. Surgery may be required if the nerve is compressed or the joint is deformed.
Medicines to treat cervical spine degeneration
Neck pain can be relieved with medication.
Pain relievers and neck stiffness:
- local anesthetic ointments, gels and patches;
- nonsteroidal anti-inflammatory drugs;
- Hormonal medications in pill form or injections into the affected joint area;
- muscle relaxants to reduce muscle spasms;
- Antidepressants to relieve chronic pain.
Treatment of cervical spondylosis without medication
Along with drug treatment, it is important for patients with cervical spondylosis to practice neck exercises. For this purpose, the person is referred to a physiotherapist for consultation. It teaches how to properly stretch and strengthen the muscles in the neck and shoulders.
Your doctor may recommend a mat or roller with metal or plastic needles. They are used for 15-30 minutes before bed to relax muscles.
Wearing a Shantz brace (neck brace) is a passive exercise therapy for the deep muscles of the neck, which are less affected by exercise. When a person wears the brace, the muscles relax, and when the brace is removed, they tense. If you wear the braces for 15-20 minutes several times a day, you can exercise and strengthen them.
It should only be worn for 2–3 hours if you have a serious neck injury. In addition, you should not lie in it, much less sleep.
Surgical treatment of cervical spine degeneration
As a rule, surgery is necessary for patients with severe spinal deformities and nerve compression.
During surgery, the surgeon will remove pathological elements (hernia, formation, etc. ) or part of the vertebrae. After such treatment, a long period of rehabilitation is required: wearing a Shants brace or stiff brace of the cervical spine, physical therapy, regular walking, taking painkillers.
Complications and consequences of cervical spine degeneration
Without treatment, the discs will gradually wear away and the vertebrae will be "erased".
Common complications of cervical spondylosis:
- intractable pain syndrome in the head, neck, and chest;
- cramps, dyskinesia and numbness in the hands;
- frequent dizziness, impaired coordination of movements, fine and gross motor skills.
Preventing degenerative changes in the cervical spine ("cervical spondylosis")
There are no specific preventative measures for true cervical spondylosis because it is a genetic disease.
To avoid the appearance of non-specific neck pain, which is mistakenly associated with cervical spondylosis, it is important to ensure correct posture and physical activity: the more a person moves, the better the condition of the muscles and bones. , ligaments and joints as possible.
To stay physically active, adults need 150 minutes of moderate-intensity aerobic activity each week. Brisk walking, swimming, cycling, tennis, dancing or rollerblading are all suitable. Pilates and yoga will help strengthen your muscles.
In addition, gymnastics helps to avoid excessive tension of the neck muscles and the appearance of pain: tilt the head forward, backward, alternately to each shoulder and rotate, as well as sleeping on an orthopedic pillow.
You should avoid cervical spine injury: do not jump upside down in the water, wear a seat belt in the car (to prevent whiplash injuries in an accident).

Sleeping position when having back pain
Pain in the neck and back, often attributed to cartilage degeneration, can be the result of an uncomfortable sleeping position.
During sleep, the head and spine should be at the same level. This position minimizes additional pressure on the neck area.
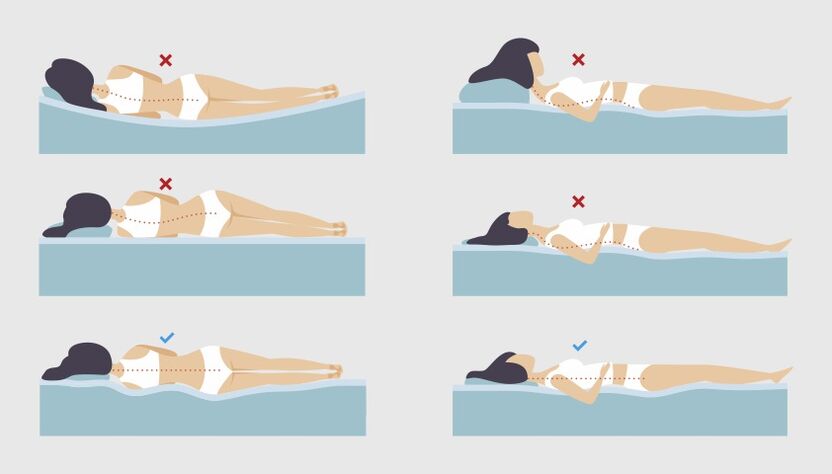
If the person sleeps mainly on their back, the average pillow height is 6–11 cm. If the person sleeps on their side, the pillow will be thicker: from 9 to 13 cm, so the desired angle will be achieved. maintained between the shoulders and head, the cervical spine will not sag, the muscles will stretch to compensate for the inconvenience.
Furthermore, the greater the person's weight, the higher the pillow. You also need to pay attention to the firmness of the mattress. The softer it is, the more it sags under the weight of the body and the higher the pillow. In addition, it is better not to always sleep on one side - this leads to muscle imbalance.
If a person likes to sleep on his stomach, he may experience back and neck pain more often. The fact is that in this position it is very difficult to keep the spine in a neutral position. To reduce stress on your back, you can place a pillow under your pelvis and lower abdomen, and choose a flat pillow under your head, or even sleep without a pillow.
Additionally, you can use special orthopedic pillows.
Frequently asked questions
- Where can the pain radiate from due to "cervical osteonecrosis"?
Pain from cervical spondylosis can spread to the shoulder or arm, and intensifies when moving or standing.
- How to reduce dizziness with cervical spondylosis?
To reduce dizziness, you should maintain a comfortable position where you are less likely to fall (sitting in a chair with a backrest or lying down) and call for help. After 5–7 minutes, you can try to turn your head again: most likely the dizziness will pass during this time. If dizziness persists or worsens, nausea, vomiting or other neurological symptoms appear (impaired speech, vision, movement, swallowing, sensitivity), you should call an ambulance. rescue as soon as possible.
- How to sleep properly when suffering from "cervical spondylosis"?
During sleep, the head and spine should be at the same level. This position minimizes additional pressure on the neck area.
- How long does the severity of cervical spondylosis last?
On average, symptoms aggravated by degenerative changes in the cervical spine ("cervical spondylosis") last 4 to 7 days. Nonsteroidal anti-inflammatory drugs and muscle relaxants are used to relieve pain. During this time, it is better for everyone to stay calm and wear a neck brace.
- Which doctor treats "osteolysis" of the cervical spine?
Diagnosis and treatment of pain in the cervical region is performed by neurologists, neurosurgeons, orthopedists and general practitioners.















































